- Free Electronic Health Record For Mac
- Free Electronic Medical Records For Mac Drivers
- Free Electronic Medical Records For Macneal
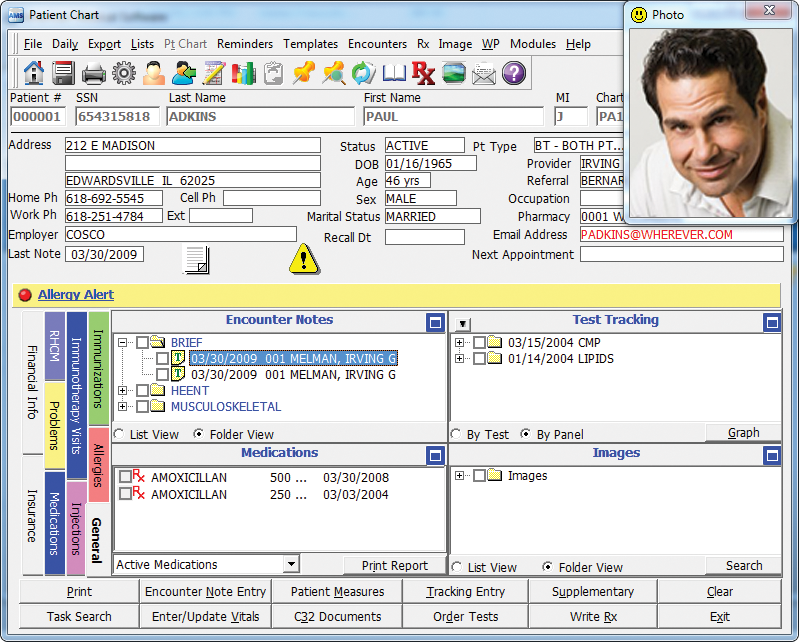
OpenEMR is a medical practice management, electronic medical records, prescription writing, and medical billing application. It is a free open source replacement for medical applications such as.
Compare electronic Mac EMR Software to find the best fit for your practice. Get free demos, price quotes and reviews of leading Mac systems. We also speak with more and more doctors who want to run medical billing software or electronic medical records (EMRs)—also often called electronic health records (EHRs)—on Macs. A Mac-native. C-CDA documents “require” a limited number of sections EHR vendors frequently support inclusion of only required sections even if information exists in the medical record for “optional” sections. The major care providers and hospitals generally use Electronic Health Record (EHR) or Electronic Medical Record (EMR) systems by a company called Epic, although there are plenty of companies that do substantially the same thing: Practice Fusion, Allscripts, athenahealth, eClinicalWorks, drchrono, and countless others.
- It comes with many features that many other practice management software packages charge extra for, including electronic medical records, electronic filing of insurance claims, and frames inventory. The only non-standard products we have is our onsite training and data conversion services.
- Electronic health records software (EHR) for specialties such as long-term care, cardiology, Chiropractic, behavioral health, internal medicine, substance abuse, nephrology, dialysis clinic must provide unique tools to streamline, manage, and document the clinical workflow of those specialists such as specifying the area of concern (for example.
- Maintain medical history records for you and your family with a great electronic medical records app. About Medical Record Medical records represent the systematic documentation of an individual's medical care and clinical history across a predefined period of time, usually under a single provider.
Abstract
Many people know of Health Level 7 (HL7) as an organization that creates health care messaging standards. Health Level 7 is also developing standards for the representation of clinical documents (such as discharge summaries and progress notes). These document standards make up the HL7 Clinical Document Architecture (CDA). The HL7 CDA Framework, release 1.0, became an ANSI-approved HL7 standard in November 2000. This article presents the approach and objectives of the CDA, along with a technical overview of the standard.
The CDA is a document markup standard that specifies the structure and semantics of clinical documents. A CDA document is a defined and complete information object that can include text, images, sounds, and other multimedia content. The document can be sent inside an HL7 message and can exist independently, outside a transferring message. The first release of the standard has attempted to fill an important gap by addressing common and largely narrative clinical notes. It deliberately leaves out certain advanced and complex semantics, both to foster broad implementation and to give time for these complex semantics to be fleshed out within HL7.
E-reader For Mac
Being a part of the emerging HL7 version 3 family of standards, the CDA derives its semantic content from the shared HL7 Reference Information Model and is implemented in Extensible Markup Language. The HL7 mission is to develop standards that enable semantic interoperability across all platforms. The HL7 version 3 family of standards, including the CDA, are moving us closer to the realization of this vision.
Health Level 7 (HL7)1 is a standards-setting organization accredited by the American National Standards Institute (ANSI). They have developed communication protocols widely used in the United States, with growing international recognition and implementations. A vendor- and provider-supported organization, its mission is to provide standards for the exchange, management, and integration of data that support clinical patient care and the management, delivery, and evaluation of health care services. This encompasses the complete life cycle of a standards specification—development, adoption, market recognition, utilization, and adherence. The HL7 specifications are unified by shared reference models of the health care and technical domains. The HL7 version 2.4 messaging standard is currently in use, and version 3, which represents several fundamental changes to the HL7 messaging approach, is in an advanced stage of development.
Many people know of HL7 as an organization that creates health care messaging standards. Health Level 7 is also developing standards for the representation of clinical documents (such as discharge summaries and progress notes). These document standards make up the HL7 Clinical Document Architecture (CDA). The HL7 Clinical Document Architecture, release 1.0, became an ANSI-approved HL7 Standard in November 2000.4
This article is intended to serve as an introduction to the CDA standard. It is geared toward medical informaticians who do not have significant familiarity with HL7 version 3, and it is intended to introduce the approach and objectives used in the creation of the standard and present an overview of the standard—not sufficient for implementation but sufficiently detailed to enable the reader to understand the scope and contents of the standard. Interested readers looking for detailed descriptions are encouraged to contact HL7 (www.hl7.org) for a copy of the normative specification.
Overview of the CDA
The need for a clinical document standard stems from the desire to unlock the considerable clinical content currently stored in free-text clinical notes and to enable comparison of content from documents created on information systems of widely varying characteristics. Given the variability in clinical notes, including structure, underlying information models, degree of semantic encoding, use of standard healthcare terminologies, and platform- and vendor-specific features, it is currently difficult to store and exchange documents with retention of standardized semantics over both time and distance. And while the current CDA standard does not fully enable these main driving objectives, it takes us a step closer.
The CDA is a document markup standard that specifies the structure and semantics of “clinical documents.” A clinical document is a documentation of observations and services and has the following defining characteristics:
Persistence. A clinical document continues to exist in an unaltered state, for a time period defined by local and regulatory requirements.
Stewardship. A clinical document is maintained by a person or organization entrusted with its care.
Potential for authentication. A clinical document is an assemblage of information that is intended to be legally authenticated.
Wholeness. Authentication of a clinical document applies to the whole and does not apply to portions of the document without the full context of the document.
Human readability. A clinical document is human readable.
Many draft and existing standards have helped inform the development of the CDA,14 and several guiding principles have driven the design:
Give priority to documents generated by clinicians involved in direct patient care. There are many requirements and uses for clinical information, such as direct patient care, outcome research, and public health reporting. The CDA will give priority to defining documents that are created by clinicians involved in direct patient care, assuming the other uses will be derivable. The CDA will define documents produced by providers seeing patients and will not define views or downstream uses of those documents.
Minimize the technical barriers needed to implement the Standard. There are estimated to be hundreds of thousands of nonstandardized clinical documents in existence. The CDA will facilitate standardization of these documents by allowing cost effective implementation across as wide a spectrum of systems as possible; by supporting exchange of human-readable documents between users, including those with different levels of technical sophistication; by enabling a wide range of post-exchange processing applications; by providing compatibility with a wide range of document creation applications; and by using non-health-care–specific standards where possible.
Promote longevity of all information encoded according to this architecture. The CDA documents will be application- and platform-independent and can be viewed and edited by a number of tools, both now and in the future.
Promote exchange that is independent of the underlying transfer or storage mechanism. The ability to exchange or store CDA documents will be application- and platform-independent. These documents can be exchanged in HL7 messages, via e-mail, on a floppy disc, etc. A CDA document can be stored as an independent file, within a document management system, within a database, etc.
Enable policy makers to control their own information requirements without extension to this specification. The CDA will define an extensibility mechanism that allows local implementations to represent information that is not formally represented in the standard.
The CDA is part of the HL7 version 3 family of standards. This family, which includes both CDA and the evolving version 3 message standards, all derive their semantic content from the shared HL7 Reference Information Model (RIM)15 and are implemented in Extensible Markup Language (XML).16 The process for generating an XML-based implementation from the RIM is part of the version 3 development methodology. The exact style of HL7's XML representation was a carefully considered balance of technical, practical, and functional considerations.18–
At the heart of the HL7 version 3 family of standards lies a shared information model, the HL7 RIM.14 An object-oriented model created as part of the version 3 methodology, the RIM is a large pictorial representation of clinical data and identifies the life cycles of events that messages and documents convey. All version 3 products derive their semantic content from the RIM. The various committees in HL7 engage in an iterative consensus process to continually refine the RIM to meet identified use cases. Figure 1▶ is a small subset of RIM version 0.98 that was used in the derivation of the CDA.
Subset of RIM version 0.98. A small subset of the HL7 Referenced Information Model, Version 0.98, used in the derivation of the CDA.
The RIM includes a new set of data types developed for use in the HL7 version 3 family of standards. These data types include some of the familiar ones used in HL7 v2.x messaging, such as STRING (ST), INTEGER (INT), and TIME STAMP (TS), as well as new data types such as ENCODED DATA (ED), which supports multimedia; INTERVAL of TIME (IVL<TS>), which allows for the expression of a time range; and CONCEPT DESCRIPTOR (CD), which supports the post-coordination of codes (or, stated in another way, the combining of codes from a terminology to create a new concept).
A CDA document is a defined and complete information object that can include text, images, sounds, and other multimedia content. The document can be sent inside an HL7 message and can exist independently outside a transferring message. There is a critical interdependence between clinical documents and document management systems. If CDA documents are viewed outside the context of a document management system, it cannot be known with certainty whether or not the viewed document is current. Clinical documents can be revised, and they can be appended to existing documents. In practice, it is impossible to guarantee an explicit forward pointer from an outdated version to the newer version. Document management systems and HL7 messages that carry CDA documents convey critical contextual information that minimizes the risk of viewing superseded information.
The “A” in “CDA”
The complete CDA will include a hierarchic set of document specifications. This hierarchy is referred to as an “architecture” (the “A” in “CDA”). This architecture, which can be thought of as a set of hierarchically related XML Document Type Definitions (DTD) or schemas,24,25 is envisioned for future releases of the CDA standard. The current CDA standard has defined only the top node of the hierarchy, known as “CDA Level One.”
Level One is sufficiently detailed to represent largely narrative clinical notes. The specification defines the document header in detail, while the document body is largely structural. Level One is intended to minimize the technical barriers to adoption of the standard while providing a gentle introduction to the RIM. It intentionally lacks some of the complex semantics that will be used in HL7 version 3 messaging (such as the ability to fully encode orders and observations). It is hoped that the provision of deeper levels of the architecture will provide a migration pathway for implementers to iteratively add greater markup to clinical documents.
Level Two is envisioned as a set of templates or constraints that can be layered on top of the CDA Level One specification. A template may, for instance, specify that a document of type “history-and-physical” will contain a mandatory “subjective” section; a mandatory “physical-examination” section containing a mandatory “vital-signs” section and an optional “cardiovascular-examination” section; and a mandatory “assessment” section followed by a “plan” section. This type of template development will require considerable domain knowledge and participation from professional societies so that created templates are widely embraced and supported. Health Level 7 is now in the process of establishing necessary liaison relationships with professional societies.
Level Three of the CDA will add additional RIM-derived markup to the CDA Level One specification, enabling clinical content to be formally expressed to the extent that is it modeled in the RIM or to the extent that it can be expressed in an HL7 version 3 message. This could, for instance, allow an order message to be extracted from a clinical document, allow for a detailed representation of symptoms and findings, and allow for billing codes to be automatically extracted.
The clinical content of CDA documents will remain invariable across all levels of the architecture. Each level both enables and enhances the standardized expression of richer shared semantics. Thus, a single report can be marked up as a Level One, Level Two, or Level Three document, and its clinical content will not vary. What will vary between the levels are the degree to which clinical content can be machine processible in an exchange context and the degree to which clinical document specifications can impose constraints on content.
Clinical Document Architecture Technical Overview
A CDA document has a header and a body. The header conveys the context in which the document was created, and the body contains the informational (factual) statements that make up the actual content of the document. The purpose of the header is to make clinical document exchange possible across and within institutions; facilitate clinical document management; and facilitate compilation of an individual patient's clinical documents into a lifetime electronic health record.
The header has four logical components:
Document information identifies the document, defines confidentiality status, and describes relationships to other documents and orders.
Encounter data describes the setting in which a documented encounter occurred
Service actors include those who authenticate the document, those intended to receive a copy of the document, document originators and transcriptionists, and health care providers who participated in the service(s) being documented
Service targets include the patient and other significant participants (such as family members).
The CDA body comprises sections, paragraphs, lists, and tables. These structural components have captions, can nest (so that, for instance, a section can contain a section), and can contain character data, multi-media, and codes drawn from standard terminologies.
Appendix 1 shows a sample clinical document, and Appendix 2 shows a CDA-encoding of that sample document. The sample CDA document includes many optional components (including some that are not explicitly shown in Appendix 1) to better illustrate more features. Line numbers in Appendix 2 are be referenced throughout this technical overview to help illustrate the described concepts.
CDA Header (Appendix 2, Lines 4–120)
Document Information (Appendix 2, Lines 5–25)
A CDA document can be an original document, an addendum to an existing document, or a revision of an existing document. An original document is the first version of a document. An addendum is an appendage to an existing report that contains supplemental information. The parent report being appended remains in place and its content and status are unaltered. A replacement report is a revision that replaces an existing report. The replacement report gets a new globally unique <id>* value but uses the same value for <set_id> as the parent report being replaced, and increments the value of <version_nbr> by 1 (Appendix 2, lines 5–7). The parent report is considered superseded but is still retained in the system for historical reference. Addendum and replacement documents reference the parent report via a <document_relationship> (Appendix 2, lines 13–20).
Pdf Reader For Mac
Documents can also be related to one or more orders. The <fulfills_order> component relates the current document to the unique identifier(s) of the orders that have been fulfilled (Appendix 2, lines 21–25) by this document.
Every document has a required document type code, <document_type_cd> (Appendix 2, lines 8–9), which classifies the document. Abbyy business card reader for mac. The externally defined vocabulary domain for <document_type_cd> is drawn from LOINC (Logical Observation Identifiers, Names and Codes).26, The creation of an ontology of clinical document names and codes in LOINC was accelerated by the contributions of the Document Ontology Task Force, a consortium of standards and vocabulary organizations sponsored by HL7 with support from the Veterans Health Administration, charged with this task. On the basis of the analysis of more than 2,000 clinical document names, the task force formulated a terminology model that was given to LOINC to guide the creation of fully specified document names.28,29
Many temporal events come into play in the creation and validation of a CDA document. Some of the relevant times are part of the document information (e.g., <origination_dttm>, which represents the time a document is initiated), while other times relate to the encounter (e.g., <encounter_tmr>), and the time during which various service actors and targets played a role (e.g., <participation_tmr>). Some temporal events can be represented as a specific point in time (indicated by an XML element name ending in “_dttm” and using the HL7 “point in time” [TS] data type), while other temporal events include time points or time intervals (indicated by an XML element name ending in “_tmr” and using the HL7 “interval of time” [IVL<TS>] or “general time specification” [GTS] data type).
The CDA header indicates document confidentiality status using the coded <confidentiality_cd> component (Appendix 2, lines 11–12).30 A single document confidentiality status indicator in the header will apply to the entire document. Alternatively, to assign different levels of confidentiality to different portions of the document, implementers can include more than one confidentiality status indicator in the header and then reference the appropriate indicator from a structure within the document body.
Encounter Data (Appendix 2, Lines 26–38)
Encounter data include an encounter identifier, an encounter time stamp, and a location. An encounter also includes an optional practice setting code, <practice_setting_cd>, which is a categorization of the clinical setting (e.g., cardiology clinic, primary care clinic, rehabilitation hospital, skilled nursing facility) in which care is delivered (Appendix 2, lines 28–29).
Service Actors (Appendix 2, Lines 39–84)
All people and organizations concerned with a CDA document can be associated with the document as either service actors (described here) or service targets (described next). Service actors include those who authenticate the document, those intended to receive a copy of the document, document originators and transcriptionists, and health care providers who participated in the services being documented. Service actors are capable of and accountable for their independent decisions.
Specific service actors defined in the CDA header include <authenticator>, <legal_authenticator> (Appendix 2, lines 39–57), <originator> (Appendix 2, lines 58–70), <intended_recipient>, <originating_ organization> (Appendix 2, lines 71–77), <transcriptionist>, and <provider> (Appendix 2, lines 78–84).
The CDA is a standard that specifies the structure of exchanged clinical documents. In a case in which a local document is transformed into a CDA document for exchange, authentication occurs on the local document and that fact is reflected in the exchanged CDA document. A CDA document can reflect the unauthenticated, authenticated, or legally authenticated state. The unauthenticated state exists when no authentication information has been recorded (i.e., tit is the absence of being either authenticated or legally authenticated). An authenticated document exists when one or more providers have attested to the accuracy of the document. A legally authenticated document exists when the person who is legally responsible for the document has attested to its accuracy. Both authentication and legal authentication require that a document be signed manually or electronically by the responsible person. Although electronic signatures are not currently part of the CDA header, the CDA header does require the acquisition of a signature to be documented via the <signature_cd> component (Appendix 2, line 42).
The CDA documents can be originated (authored) by human beings or machines, or both. The <originator> element is used to indicate human origination (Appendix 2, lines 58–70), and the <originating_device> element is used to indicate machine origination (Appendix 2, lines 105–16). The CDA header requires the specification of one or more document originators but does not require that there be a human originator.
Intended recipients, indicated by <intended_recipient>, are those people to whom a copy of the document is to be sent. The CDA header can specify the organization from which the document originates and that is in charge of maintaining the document using the <originating_organization> component (Appendix 2, lines 71–77). The CDA header requires the specification of one or more health care providers, indicated by <provider>, who participated in the services being documented (Appendix 2, lines 78–84).
Service Targets (Appendix 2, Line 85-116)
Service targets are physical entities, including living subjects and inanimate material, that are typically the object of services being documented. Service targets include the patient and other significant participants (such as family members).
The CDA header requires one and only one value for <patient> (Appendix 2, lines 85–104). The value of the <patient> component indicates whose medical record this document belongs to. By default, the <patient> is also the principal subject of the services being documented. The <patient> is defined as having the same components as any other person, plus a date of birth, <birth_dttm> (Appendix 2, line 102), and a gender, <administrative_gender_cd> (Appendix 2, line 103).
In addition to <patient>, other people (e.g., a patient's child, parent, beneficiary) may play a role in certain circumstances or with certain types of documents. The CDA header can specify one or more of these people via the <service_target> component.
CDA Body (Appendix 2, Line 121-268)
Document Structures
The CDA body comprises “structures” that include sections, paragraphs, lists, and tables. These structures have captions, can nest (so that, for instance, a section can contain a section), and can contain “entries” such as character data, multimedia, and codes drawn from standard terminologies.
All CDA structures have a “context,” meaning that attribution assigned to a structure is applicable to the contents contained in that structure, and are inherited by nested structures unless overridden. Structure attributes of a CDA include confidentiality, origination, and human language (Figure 2▶).
Structure “context” in CDA body. Attribution ascribed to structural components in the CDA Body (sections, paragraphs, lists, tables) define the structure's “context”. These attributes are applicable to the contents of the structure, and are inherited by nested structures, unless overridden.
The confidentiality attribute and the originator attribute reference values are expressed in the CDA header (using the XML “IDREFS” data type). The confidentiality attribute references the <confidentiality_cd> component (Appendix 2, line 121), whereas the originator attribute references the <originator> or the <originating_device> component (Appendix 2, line 227). Thus, all applicable confidentiality and originator values are expressed in the CDA header and referenced by structures in the body. The language attribute is used to indicate the human language of character data and is specified using the “xml:lang” attribute as defined in the XML 1.0 Recommendation:
A special attribute named xml:lang may be inserted in documents to specify the language used in the contents and attribute values of any element in an XML document. In valid documents, this attribute, like any other, must be declared if it is used. The values of the attribute are language identifiers as defined by the IETF (Internet Engineering Task Force) RFC 1766: Tags for the Identification of Languages, ed. H. Alvestrand, 1995.
A CDA structure has a caption, <caption> (Appendix 2, lines 123–126), which is an optionally coded heading or label for a container. The vocabulary domain used to codify a caption (Appendix 2, line 124) is externally defined by LOINC. The creation of section codes in LOINC was facilitated by input from the Document Ontology Task Force.10,28,29,31
The CDA <list> is patterned after the HTML list structure and contains one or more <item> elements (Appendix 2, lines 138–142). The list_type attribute specifies whether the <list> is ordered or unordered, with unordered being the default. An ordered list is used when the ordering of list items is meaningful. The CDA <table> is a modification of the XHTML table model, which has removed some of the formatting tags. In the CDA body, any information can be presented as a table. The table markup is for presentation purposes only and, unlike a database table, does not possess meaningful field names.
In general, CDA structures are similar to HTML structures. Because of the similarity, transforming CDA structures into HTML structures for the sake of viewing a CDA document on a Web browser is very straightforward, and CDA documents can be authored using tools that generate HTML. The resulting HTML can be transformed into CDA. It should be noted that HTML will not support much of the detailed markup in the CDA, but it is expected to retain compatibility with the structural components even as the CDA standard evolves.
Document Entries
Document entries in a CDA occur in structures and include character data; coded entries, <coded_entry>; a recursively nesting wrapper, <content>; a generic referencing mechanism, <link>; and multimedia, <observation_media>.
The CDA element <coded_entry> (Appendix 2, lines 239–242) is used to insert codes from HL7-recognized coding schemes into CDA documents. The <content> element (Appendix 2, lines 236–243) can be thought of as a fine-grained wrapper and explicit anchor. Because it can nest recursively, the <content> element enables wrapping a string of plain text down to as small a chunk as desired. Coded entries can reference these <content> anchors to indicate the original text that supports the use of the code, in a manner similar to that described by Friedman et al. The process is shown in Figure 3▶. In the first case, <coded_entry> is used to simply insert a code into a CDA document, without referencing the original text. In the second case, <coded_entry> explicitly references the original text that supports the assigned code.
Referencing original text with <coded_entry>. In the first case, <coded_entry> is used to simply insert a code into a CDA document, without referencing the original text. In the second case, <coded_entry> explicitly references the original text that supports the assigned code.
The primary intent of <coded_entry> is to facilitate document indexing, search, and retrieval and to provide a standard convention for insertion of locally meaningful codes. The CDA body lacks a robust semantic for the full representation of a code's context. Thus, when a computer encounters a code for “chest pain” occurring in a “history of present illness” section, the computer cannot reliably determine whether “chest pain” refers to the patient or to the patient's family member, nor can it reliably determine whether “chest pain” is present or stated to be absent. For now, these determinations rely on human interpretation. As consensus on these issues develops within HL7, the shared understanding will be reflected in the RIM, and they will be incorporated into CDA.
Modifiers of coded entries (e.g., Mass :: Has-color :: Blue; Mass :: Has-shape :: Round) can be formally expressed using the power of the coded entry's Concept Descriptor (CD) data type, which allows for post-coordination, or the combining of codes from a terminology to create a new concept. The use of post-coordination raises some interesting challenges in data extraction, since many concepts that exist in the underlying terminology (such as “nodule-of-skin”) can also be constructed via post-coordination (“lesion-of-skin :: Has-morphology :: nodule”). While the approach to this challenge is outside the scope of the current paper, it is of active and ongoing interest to HL7.
The CDA <link> is a generic referencing mechanism, similar to the HTML anchor tag. Several groups (such as the World Wide Web Consortium) are actively developing formal link specifications.35 When a suitable open standard is available and implemented, it will be reviewed with the intent to incorporate it into the CDA specification. The <observation_media> element (Appendix 2, lines 194–198) represents media that is logically a part of a CDA document but is stored outside the document and incorporated by reference, in a manner similar to the HTML image tag.
Localization and Transformation issues
Those implementing structured document systems for health care may choose to adopt CDA directly into their application or environment or may implement their own internal document representation standards. In the first case, local implementations of CDA will often require the ability to extend or localize the shared semantics expressed by CDA. In the second case, exchange of CDA documents will require that local document instances be transformed into CDA-compliant instances.
The implementation of localization in CDA parallels the “version compatibility definition” in HL7 V2.x that enables new fields, segments, and components to be introduced at the tail end of the normative specification. In the process of creating the CDA XML DTD, the CDA specification adds a <local_header> element to the end of every XML content model in the header (Appendix 2, lines 117–119) and a <local_markup> element to the end of every XML content model in the body. These localization tags are optionally repeating and recursive. The “descriptor” attribute describes the element, and the value can be drawn from a local vocabulary domain. The “ignore” attribute tells the receiver to ignore just the local tag (ignore=”markup”) or to ignore the tag and all contained content (ignore=”all”).
Transformation of locally defined document instances into CDA-compliant instances can be performed with special-purpose SGML36,37 and XML transformation languages (such as Hytime Architectural Forms,12 Document Style Semantics and Specification Language,38 and Extensible Stylesheet Language39) or with general programming languages. Where possible, local semantics should be mapped into the CDA's shared semantics. In the case where local semantics have not been standardized in CDA, mapping to CDA's <local_header> or <local_markup> is appropriate.
Each transformation language has potential syntactic limitations in the type of mappings that can be formally expressed. In addition, there are semantic mappings that cannot be resolved regardless of the transformation language employed. Although the discussion here focuses on mapping from one DTD to another, the issues are no different from those that arise in the more general sense of mapping from one information model to another. Elements in the local instance may be in different order than in CDA (e.g., <dob> <name> vs. <person_name> <birth_dttm>). The source may be missing a required element (e.g., CDA requires a globally unique document identifier). The source and CDA may have different vocabulary domains (e.g., “male” vs. “M”). Elements may have different data types (e.g., “January 13, 1923” vs. “1923-01-13”). The source may be have coarser granularity (i.e., less detailed markup) than CDA (e.g., <name> Henry Levin, the 7th </name> vs. <person_name> <GIV V=”Henry”/> <FAM V=”Levin”/> <SFX V= ”the 7th”/> </person_name>).
It is likely that transformation issues will be minimized to the extent that the CDA specifications and the underlying RIM are unambiguous. Where local requirements not met by the CDA are identified, they should be considered candidate proposals to enhance HL7 or CDA semantics.
Conclusion
The first release of the ANSI-approved HL7 CDA represents the culmination of close to four years of effort. With this standard, HL7 has entered the realm of defining the structure and semantics of clinical documents. This first standard has attempted to fill a huge gap by standardizing common clinical notes such as history and physicals, discharge summaries, and progress notes. It deliberately leaves out certain advanced and complex semantics both to foster broad implementation and to give time for these complex semantics to be flushed out in the RIM. Health Level 7 is currently balloting the new version 3 messaging specifications; as a result, considerable energy is going into refining the RIM. It is expected that future releases of CDA will include deeper layers of the architecture that encode richer semantics and that the current standard will serve as a stepping stone, allowing users to implement these releases progressively.
More and more, decision support applications will communicate with electronic health records via an HL7 interface. For this transfer of information to be rich, detailed, and unambiguous, a high degree of semantic interoperability between applications is needed. The HL7 version 3 family of standards, including the CDA, are moving us closer to the realization of this vision.
Acknowledgments
They also thank Jonathan Lukoff, MD, William W. Stead, MD, and the JAMIA reviewers for their critique of the manuscript.
Appendix A: Sample Document
Appendix B: Sample CDA Document
This CDA document uses rich markup to illustrate many features of CDA. Many of the elements included in this sample are optional. This is a validated CDA document that conforms to the Standard.
Footnotes
*In this text, XML element names that are in the CDA standard are surrounded by angle brackets (< >).
References
Free Electronic Health Record For Mac